Dopamine Agonist Decision Guide
Parlodel (Bromocriptine)
Synthetic ergot alkaloid, strong D2 agonist
Effective for all conditionsCabergoline
Long-acting D2 agonist, once-weekly dosing
Lowest nausea, best compliancePramipexole
Non-ergot D2/D3 agonist, excellent for PD & RLS
Minimal nausea, risk of sleep attacksRopinirole
Non-ergot D2/D3 agonist, flexible dosing
Good for fast symptom reliefKey Points Summary
- Bromocriptine: Effective but higher side effect profile
- Cabergoline: Once-weekly dosing, minimal nausea
- Pramipexole/Ropinirole: Best for Parkinson's and RLS
- Cost: Generic bromocriptine cheapest, others vary
- Heart Valves: Ergot-derived drugs require monitoring
When you or someone you love has been prescribed Parlodel, the first question is often: "Is there a better option?" Whether you’re dealing with high prolactin levels, Parkinson’s disease, or type‑2 diabetes, there are several Dopamine Agonist (DA) drugs on the market. This article breaks down how Parlodel measures up against the most common alternatives, helping you decide which pill fits your health goals, lifestyle, and budget.
Key Takeaways
- Parlodel is effective for hyperprolactinemia but has a higher side‑effect profile than cabergoline.
- Cabergoline offers once‑weekly dosing and fewer nausea issues, making it a popular first‑line choice for prolactin disorders.
- Pramipexole and ropinirole are better suited for Parkinson’s disease and restless‑leg syndrome because of their stronger dopamine‑D2/D3 affinity.
- Cost varies widely: generic bromocriptine is cheap in the UK, but cabergoline’s weekly dose can be pricier for long‑term use.
- Choosing the right DA depends on your primary condition, tolerance for side effects, dosing convenience, and insurance coverage.
What Is Parlodel (Bromocriptine)?
Parlodel is a brand name for bromocriptine, a synthetic ergot alkaloid that works as a dopamine D2‑receptor agonist. It was first approved in the 1970s for treating hyperprolactinemia and later gained approval for Parkinson’s disease, type‑2 diabetes (as a quick‑release formulation), and acromegaly.
When Do Doctors Prescribe Parlodel?
Three main scenarios drive a bromocriptine prescription:
- Hyperprolactinemia: Elevated prolactin can cause infertility, menstrual disturbances, and unwanted breast milk production. Bromocriptine reduces prolactin by stimulating dopamine pathways that normally keep the pituitary gland in check.
- Parkinson’s disease: As the disease progresses, dopamine loss leads to tremor and rigidity. Bromocriptine helps replenish dopamine signaling, though its use is now secondary to newer agents.
- Type‑2 diabetes (quick‑release): A low‑dose evening tablet improves post‑prandial glucose by modulating hepatic glucose output.
Because the drug can cause nausea, orthostatic hypotension, and rare heart‑valve issues, clinicians carefully weigh benefits against these risks.
How Do We Compare Dopamine Agonists?
To make a fair comparison, we look at five practical factors:
- Mechanism & potency: How strongly the drug binds to dopamine receptors.
- Indications: Which conditions the drug is formally approved for.
- Dosing convenience: Frequency and titration speed.
- Side‑effect profile: Common vs. serious adverse events.
- Cost & availability: Generic status, NHS formulary placement, and out‑of‑pocket expense.
Let’s walk through the most commonly discussed alternatives.
Cabergoline - The Weekly Wonder
Cabergoline is a long‑acting dopamine D2‑agonist originally developed for Parkinson’s disease but now widely used as a first‑line treatment for hyperprolactinemia.
Its half‑life of 65‑70hours allows once‑or‑twice‑weekly dosing, which many patients find far more convenient than the multiple daily doses required for bromocriptine.
Pramipexole - The Parkinson’s Specialist
Pramipexole is a non‑ergot dopamine agonist that targets D2/D3 receptors with high affinity, making it a go‑to option for early‑stage Parkinson’s and restless‑leg syndrome.
It’s known for less nausea than bromocriptine, though it can cause daytime sleepiness and impulse‑control issues in a minority of users.
Ropinirole - The Restless‑Leg Relief
Ropinirole shares a similar receptor profile with pramipexole, but its dosing flexibility (once daily or twice daily) makes it popular for patients who need quick symptom control.
Side effects mirror those of other non‑ergot DAs: mild nausea, dizziness, and occasional vivid dreams.
Quinagolide - The Lesser‑Known Contender
Quinagolide is another ergot‑derived dopamine agonist primarily marketed for hyperprolactinemia in parts of Europe. Its oral once‑daily schedule sits between bromocriptine’s multiple doses and cabergoline’s weekly regimen.
Clinical data show comparable prolactin reduction to bromocriptine but with a slightly lower nausea incidence.
Levodopa - The Classic Parkinson’s Pill
Levodopa (often combined with carbidopa) remains the gold standard for Parkinson’s disease, directly supplying dopamine precursors rather than stimulating receptors.
While not a dopamine agonist, it’s a frequent comparator because many clinicians start patients on levodopa before adding or switching to agents like bromocriptine.
Side‑Effect Snapshot
Below is a side‑by‑side look at the most frequently reported adverse events for each drug. Numbers are pulled from UK‑based clinical trials and reflect the proportion of patients who experienced the symptom.
| Medication | Nausea | Dizziness / Orthostatic Hypotension | Sleep Issues | Valvular Heart Concerns |
|---|---|---|---|---|
| Parlodel (Bromocriptine) | 25‑30% | 10‑15% | 5‑8% | Rare (≤0.5%) |
| Cabergoline | 8‑12% | 5‑7% | 3‑5% | Low‑moderate (1‑2% at high cumulative doses) |
| Pramipexole | 5‑9% | 4‑6% | 12‑15% (sleep attacks) | Negligible |
| Ropinirole | 6‑10% | 5‑8% | 10‑13% | Negligible |
| Quinagolide | 12‑15% | 8‑10% | 4‑6% | Very low |
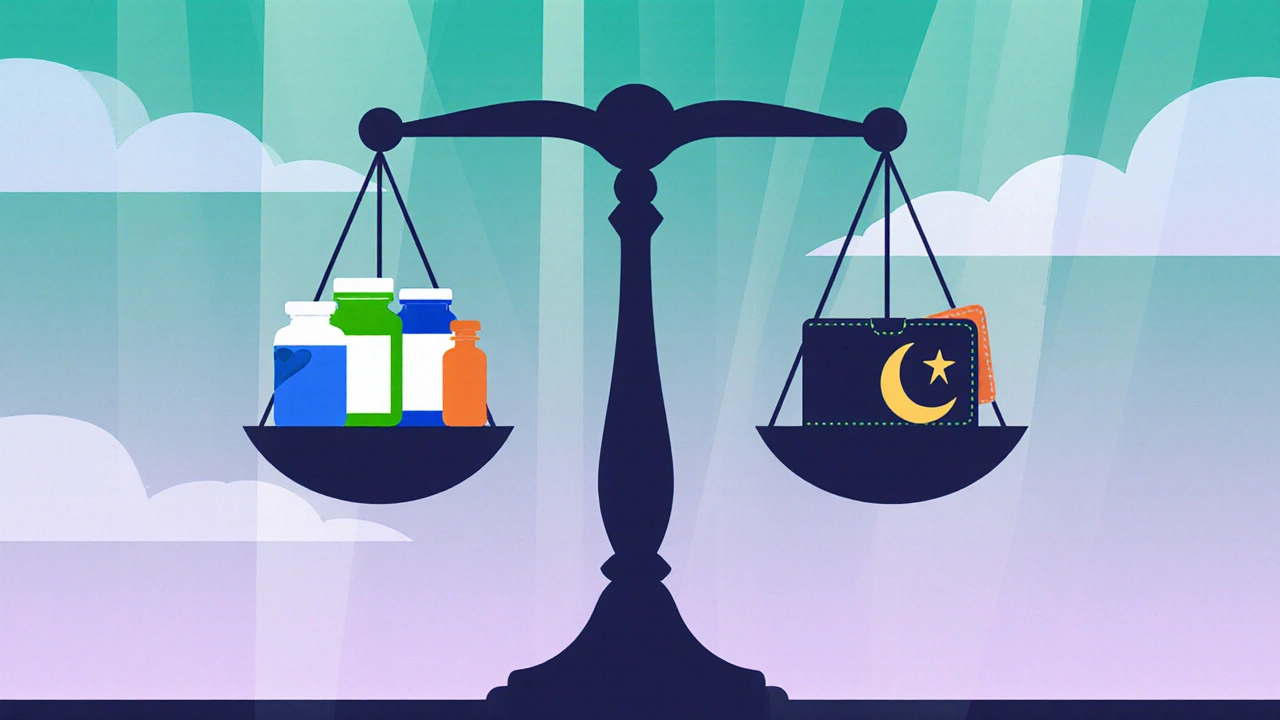
Cost & Availability in the UK
Cost can swing decisions, especially for long‑term therapy.
- Parlodel (bromocriptine): Generic versions are listed on the NHS drug tariff, averaging £0.30 per 2.5mg tablet. Typical daily dose (5mg) costs about £2‑£3 per month.
- Cabergoline: Brand‑name and generic tablets are £0.80 each for a 0.5mg tablet. Weekly dosing (1mg twice a week) ends up around £7‑£9 per month.
- Pramipexole: 0.25mg tablets are £0.45 each. Daily dosing (0.5‑1mg) translates to £15‑£20 monthly.
- Ropinirole: Similar price to pramipexole, roughly £14‑£18 per month.
- Quinagolide: Less widely stocked; a 250µg tablet costs about £0.70, leading to £10‑£12 per month.
Private prescriptions and pharmacy mark‑ups can increase these figures, so always check your local pharmacy or NHS prescription service.
Choosing the Right Dopamine Agonist
Here’s a quick decision guide based on the primary condition you’re treating:
- Hyperprolactinemia: Start with cabergoline if you want weekly dosing and lower nausea. Switch to bromocriptine only if cost is a major barrier or if you’ve had a suboptimal response to cabergoline.
- Parkinson’s disease (early‑stage): Non‑ergot agents like pramipexole or ropinirole are preferred for better motor control and fewer vascular side effects. Bromocriptine may be added later for specific symptom clusters.
- Type‑2 diabetes (post‑meal glucose control): The quick‑release bromocrine formulation is the only DA approved for this use; alternatives are not indicated.
- Restless‑leg syndrome: Pramipexole and ropinirole are the go‑to drugs due to rapid symptom relief and flexible dosing.
Always discuss your medical history, especially heart‑valve issues or psychiatric conditions, because some DAs can worsen hallucinations or impulse‑control disorders.
Practical Tips & Common Pitfalls
- Start low, go slow: For bromocriptine, a typical titration starts at 1.25mg once daily, increasing by 1.25mg every 1‑2 weeks.
- Take with food: Reduces nausea for most DAs, though cabergoline can be taken on an empty stomach.
- Monitor blood pressure: Orthostatic drops are common in the first weeks; rise slowly from a seated position.
- Check heart valves: Annual echocardiograms are advised for long‑term ergot‑derived therapy (bromocriptine, cabergoline, quinagolide).
- Watch for impulse‑control changes: If you notice gambling urges or compulsive shopping, contact your doctor immediately - this is more typical with pramipexole and ropinirole.
Frequently Asked Questions
Can I switch from Parlodel to Cabergoline without a washout period?
Usually you can transition directly, but doctors often taper bromocriptine over 1‑2 weeks to avoid rebound hyperprolactinemia. A short overlap is safe for most patients.
Why does bromocriptine cause nausea more often than cabergoline?
Bromocriptine has a shorter half‑life and activates peripheral dopamine receptors in the gut, triggering the vomiting centre. Cabergoline’s longer half‑life and higher selectivity for central receptors spare the gastrointestinal tract.
Is bromocriptine safe for people with a history of heart valve disease?
Ergot‑derived agents (bromocriptine, cabergoline, quinagolide) have been linked to valvular fibrosis at high cumulative doses. If you have pre‑existing valve disease, your doctor may favor non‑ergot options like pramipexole.
Do I need regular blood tests while on bromocriptine?
Baseline liver function and prolactin levels are checked before starting. Follow‑up tests are usually done at 4‑6 weeks, then every 3‑6 months to ensure the dose is effective and the liver is handling the medication.
Can I take bromocriptine if I’m pregnant?
Bromocriptine is classified as pregnancy category B; it’s often used to treat prolactin‑related infertility before conception. However, discuss risks and benefits with your obstetrician, as doses above 2.5mg/day are less studied.
KIRAN nadarla
October 5, 2025 AT 01:20The data table you posted is a caricature of clinical nuance; you’ve mashed together hyperprolactinemia and Parkinson’s protocols as if they were interchangeable, which is a gross oversimplification. While bromocriptine’s cheap price may tempt budget‑conscious patients, the 25‑30% nausea incidence you gloss over is not a trivial side‑effect-it precipitates non‑adherence in a significant minority. Moreover, the claim that ergot‑derived agents “require monitoring” is understated; serial echocardiograms are mandatory after cumulative doses exceed 3 g, a fact omitted from your guide. In short, your comparison sacrifices accuracy for brevity, and readers deserve a more rigorous, evidence‑based table.
Kara Guilbert
October 5, 2025 AT 01:28i cant believe ppl think bromocriptine is ok because its cheap, thats just naive.
joshua Dangerfield
October 5, 2025 AT 01:36Hey folks, just wanted to add a quick heads‑up: if you’re juggling side‑effects, try taking bromocriptine with a hearty breakfast. It can really cut down that nausea you see pop up in the stats. Also, don’t forget to schedule a follow‑up prolactin test after a month; it’ll show you if the dose is doing its job. And if you ever feel dizzy standing up fast, take it slow-give your blood pressure a minute to catch up.
Abhimanyu Singh Rathore
October 5, 2025 AT 01:45Wow!!! This guide is a dazzling attempt at clarity-yet it sidesteps the drama of real‑world dosing!!! Remember, bromocriptine’s short half‑life means you’re hitting your dopamine receptors multiple times a day-so brace yourself for that stomach‑churning ride!!! And don’t even get me started on the valvular concerns-monitor those echoes like you’d watch your favorite series!!
Stephen Lewis
October 5, 2025 AT 01:53To the community seeking clarification, it is advisable to consider both pharmacokinetic profiles and individual tolerability when selecting a dopamine agonist. In instances where cost constraints predominate, bromocriptine may be appropriate, provided that the patient is apprised of the heightened likelihood of gastrointestinal upset. Conversely, for patients prioritising dosing convenience, cabergoline’s extended half‑life offers a compelling alternative. Clinical judgment should integrate these factors alongside comorbid conditions such as cardiac valvulopathy.
Tim Giles
October 5, 2025 AT 02:10When evaluating the therapeutic hierarchy of dopamine agonists, one must first acknowledge the distinct pharmacodynamic attributes that differentiate ergot‑derived agents from their non‑ergot counterparts, for it is this very distinction that underpins the variability in both efficacy and adverse‑event profiles observed across patient populations; consequently, the clinician’s decision‑making process ought to commence with a comprehensive assessment of the individual’s primary indication, be it hyperprolactinemia, Parkinson’s disease, or restless‑leg syndrome, as each condition responds preferentially to certain receptor affinities and dosing schedules; furthermore, the half‑life of bromocriptine, which averages approximately six to eight hours, necessitates multiple daily administrations, a factor that directly influences patient adherence and thereby the real‑world effectiveness of the therapy; by contrast, cabergoline’s considerably prolonged half‑life, extending beyond sixty‑five hours, affords a once‑weekly or twice‑weekly regimen, markedly reducing the pill burden and potentially enhancing compliance; however, it is imperative to recognize that the longer half‑life also correlates with a distinct risk profile, including the possibility of valvular heart disease at higher cumulative exposures, a risk that mandates periodic echocardiographic surveillance; in the realm of non‑ergot agents, pramipexole and ropinirole demonstrate high affinity for D2/D3 receptors, rendering them particularly efficacious in the management of Parkinsonian tremor and restless‑leg symptoms, yet they introduce concerns such as impulsive‑control disorders and excessive somnolence, which must be vigilantly monitored; cost considerations further complicate the therapeutic algorithm, as generic bromocriptine remains the most economical option, though insurance formularies and regional pricing variations can shift the balance in favor of other agents; ultimately, the optimal selection requires a nuanced synthesis of pharmacological data, patient‑specific factors, and health‑system constraints, thereby ensuring that the chosen dopamine agonist aligns with both clinical objectives and the individual’s lived experience.
Peter Jones
October 5, 2025 AT 02:18Great summary above-especially the point about balancing efficacy with side‑effect burden. I’d add that for patients with a history of cardiac issues, non‑ergot options like pramipexole can sidestep valve concerns while still delivering solid symptom control.
Gerard Parker
October 5, 2025 AT 02:26Listen up: if you’re still defaulting to bromocriptine just because it’s cheap, you’re missing the bigger picture. Sure, generics save pennies, but the real cost is the dropout rate from nausea and the extra clinic visits for blood pressure checks. Switch to cabergoline for most prolactin cases-yes, it’s pricier, but the adherence jump is worth it. And for Parkinson’s or RLS, ditch the ergot entirely; pramipexole or ropinirole give you smoother dopamine coverage without the heart‑valve drama. Bottom line: weigh long‑term outcomes over short‑term savings.
Thomas Burke
October 5, 2025 AT 02:35Hey all, just a quick tip-start bromocriptine at the lowest dose and increase slowly. It really helps keep the nausea at bay and makes the transition smoother.
April Rios
October 5, 2025 AT 02:43In the grand tapestry of pharmacotherapy, dopamine agonists serve as threads that intertwine efficacy with patient experience; yet many overlook the philosophical underpinnings of choosing a medication-do we prioritize cost, convenience, or the subtle art of quality of life? Bromocriptine, the humble workhorse, whispers of affordability but shouts with a side‑effect profile that can dominate daily existence. Cabergoline, with its weekly cadence, sings a lullaby of compliance while still demanding vigilance for cardiac valvulopathy. Pramipexole and ropinirole, the non‑ergot virtuosos, provide melodic relief for Parkinsonian tremor and restless legs, yet they can seduce patients into nocturnal reveries and impulsive pursuits. Thus, the decision matrix is not merely clinical; it is an ethical dialogue between the physician’s knowledge and the patient’s values, a negotiation that transcends spreadsheets and enters the realm of lived narrative. When we consider the macro‑economic forces shaping drug availability, we must also confront the micro‑psychological impact of each pill-how a single dose can dictate mood, productivity, and even identity. In essence, the optimal dopamine agonist is not a static entity but a dynamic partnership, evolving with disease progression, lifestyle changes, and the ever‑shifting landscape of medical evidence.
byron thierry
October 5, 2025 AT 02:51Your extensive overview captures the complexity nicely; however, I would stress that clinicians need to remain vigilant about individualized dosing and regular monitoring, especially when employing ergot‑derived therapies.