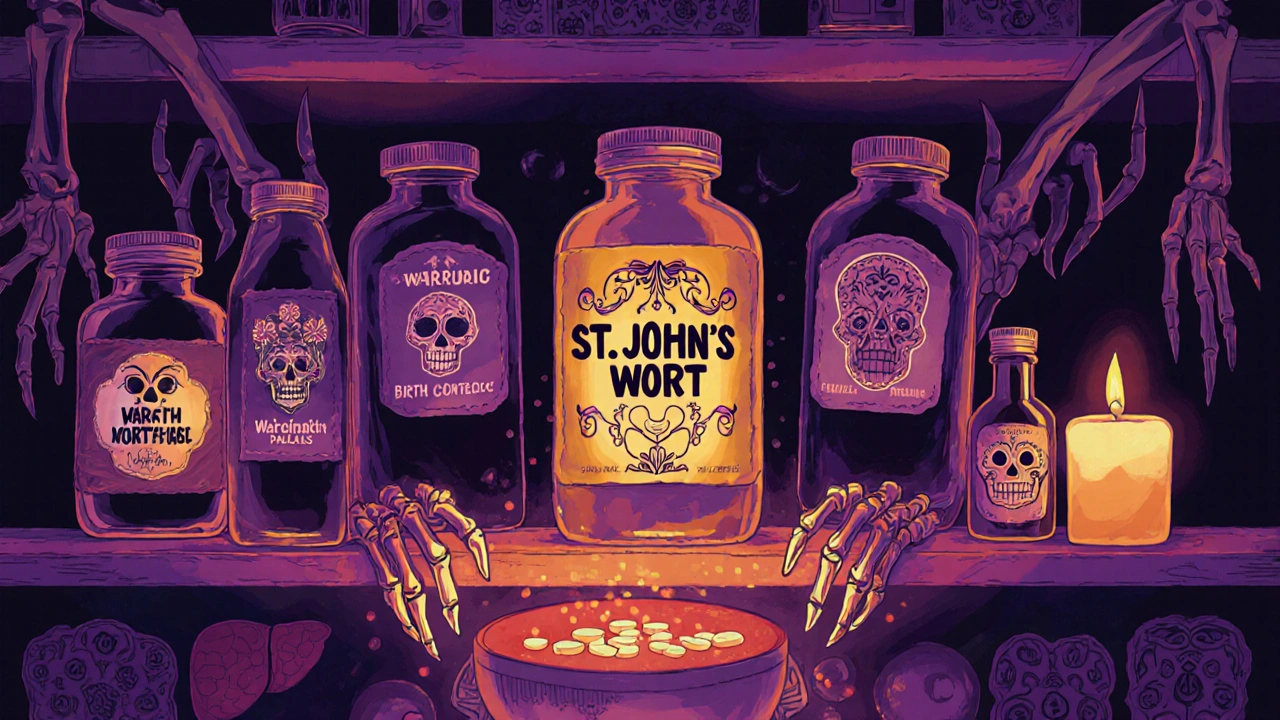
Many people turn to St. John’s Wort because they want a natural way to feel better-especially if they’re dealing with mild depression. It’s sold in pharmacies, health stores, and online as a supplement, often labeled "natural" or "herbal." But here’s the truth: St. John’s Wort isn’t harmless just because it comes from a plant. In fact, it can turn your prescription drugs into useless pills-or worse, make them dangerous.
How St. John’s Wort Changes How Your Body Handles Medication
St. John’s Wort doesn’t just float around your body doing nothing. Its main active ingredient, hyperforin, wakes up enzymes in your liver and gut that are supposed to break down drugs. These enzymes, especially CYP3A4 and CYP2C9, are like the body’s cleanup crew for medications. When St. John’s Wort turns them on full blast, your body gets rid of other drugs way faster than it should.
That means if you’re taking warfarin for blood thinning, your INR levels can crash from 2.5 down to 1.3 in less than a week. That’s not just a number-it’s the difference between being protected from a stroke and having a dangerous clot form. The same thing happens with cyclosporine, the drug transplant patients rely on to keep their new organs from being rejected. One case report showed a patient’s cyclosporine levels dropped 40% after just two weeks of St. John’s Wort. Their doctor said they were hours away from organ rejection.
It’s not just liver enzymes. St. John’s Wort also pushes out drugs from cells using a transporter called P-glycoprotein. This affects drugs like digoxin (used for heart failure) and certain HIV medications. If your body flushes out these drugs too quickly, they stop working-and that can be life-threatening.
Medications That Can Become Ineffective (or Dangerous) with St. John’s Wort
There are over 50 prescription drugs known to interact badly with St. John’s Wort. Here are the most critical ones:
- Anticoagulants (warfarin, phenprocoumon): Risk of blood clots, stroke, or pulmonary embolism.
- Immunosuppressants (cyclosporine, tacrolimus): Risk of organ rejection in transplant patients.
- HIV medications (protease inhibitors like saquinavir, NNRTIs like efavirenz): Risk of treatment failure and drug-resistant virus.
- Antidepressants (SSRIs like sertraline, fluoxetine, and nefazodone): Risk of serotonin syndrome-a potentially fatal condition with high fever, seizures, confusion, and muscle rigidity.
- Oral contraceptives: Breakthrough bleeding, unintended pregnancy-even if you take your pill perfectly.
- Anticonvulsants (phenytoin, carbamazepine): Risk of seizure breakthrough in epilepsy patients.
- Benzodiazepines (alprazolam, diazepam): Reduced anxiety control, increased panic attacks.
- Statins (simvastatin, atorvastatin): Higher risk of heart attack due to lower cholesterol control.
- Theophylline: Risk of asthma flare-ups.
- Opioids (oxycodone, fentanyl): Reduced pain relief, possible withdrawal symptoms.
And here’s the kicker: not all statins are affected the same way. Pravastatin and fluvastatin don’t interact much because they’re processed differently. But if you’re on simvastatin or atorvastatin, you’re at risk. You can’t guess-your doctor needs to check.
Why People Don’t Realize the Danger
A 2022 Johns Hopkins study surveyed 250 people taking prescription meds and using St. John’s Wort. Forty-one percent didn’t tell their doctor. Why? Because they didn’t think of it as a "medication."
"I just take a little herb for my mood," one user said on Reddit. Another wrote on Drugs.com: "I took St. John’s Wort with my birth control. I didn’t think it would do anything. Now I’m pregnant."
Even worse, people assume "natural" means "safe." But the FDA doesn’t regulate supplements like drugs. That means there’s no guarantee how much hyperforin is in your bottle. One brand might have 0.1%, another 3%. That’s a 30-fold difference. And if you stop taking St. John’s Wort suddenly, your enzyme levels don’t snap back. It can take up to two weeks for your body to reset. That’s why switching off St. John’s Wort can be just as risky as starting it.
Real Stories, Real Consequences
On HealthUnlocked, a transplant patient wrote: "My cyclosporine levels dropped 40%. My doctor said I was hours away from rejection. I didn’t know herbal supplements could do that."
A pharmacist in Glasgow shared a case from last year: a 58-year-old woman on warfarin started St. John’s Wort for low mood. Her INR dropped from 2.8 to 1.5 in 10 days. She had a minor stroke. She survived-but lost mobility in her right arm.
And then there’s the serotonin syndrome risk. Six cases were reported in Australia alone between 2000 and 2020, all involving people mixing St. John’s Wort with SSRIs. Symptoms started within 3 to 7 days: agitation, sweating, tremors, high fever. One patient needed intensive care.
These aren’t rare outliers. They’re predictable outcomes of a known mechanism.
What You Should Do If You’re Taking St. John’s Wort
If you’re on any prescription medication, don’t stop taking it. But do this:
- Ask yourself: Am I taking anything for depression, anxiety, blood thinning, heart disease, HIV, seizures, or birth control? If yes, St. John’s Wort could be interfering.
- Tell your doctor. Don’t wait for them to ask. Say: "I’m taking St. John’s Wort for my mood." Many doctors won’t ask unless you bring it up.
- Don’t quit cold turkey. If you’ve been taking it for weeks, stopping suddenly can cause withdrawal-headaches, dizziness, nausea. Talk to your doctor about a slow taper.
- Get tested. If you’re on warfarin, cyclosporine, or anticonvulsants, ask for a blood test 3-5 days after starting or stopping St. John’s Wort.
- Look for alternatives. For mild depression, therapy, exercise, and sunlight are proven to help-with zero interaction risks.
And if you’re thinking about starting St. John’s Wort? Stop. The American Psychiatric Association’s 2023 guidelines no longer recommend it for anyone taking prescription meds. Not even "sometimes." Not even "if I’m careful."

What About the People Who Say It Works?
Yes, some people report feeling better. WebMD has over 1,200 reviews, and 68% say it helped their depression. One user wrote: "My PHQ-9 score dropped from 18 to 7 in six weeks. No side effects."
That’s real. But here’s what they didn’t say: "I’m not on any other meds." Or: "I’ve been monitoring my INR every week." Or: "My doctor knows and approved this."
St. John’s Wort might help mood-but only if you’re not taking anything else that matters. If you are, the risk isn’t worth it.
The Bottom Line
St. John’s Wort isn’t a gentle herb. It’s a powerful biochemical disruptor. It can make your blood thinner useless, your transplant fail, your birth control stop working, or your antidepressant turn into a poison. It doesn’t care if you call it "natural." It doesn’t care if you bought it at the grocery store.
If you’re on any prescription drug-especially for heart, brain, immune, or mental health-St. John’s Wort is not safe for you. Even if you feel fine now. Even if you’ve taken it for months. The damage builds quietly.
There are safer ways to support your mood. Talk therapy. Regular walks. Light therapy. Omega-3s. Sleep hygiene. These don’t come with warning labels. They don’t require blood tests. And they won’t put your life at risk.
Don’t risk your health for a supplement that’s been called "one of the most dangerous herbs in modern medicine" by experts. Your body doesn’t need another herb. It needs you to be informed.
Can I take St. John’s Wort if I’m not on any medications?
If you’re not taking any prescription drugs, over-the-counter medications, or other supplements, St. John’s Wort may be low-risk for you. But even then, side effects like upset stomach, dizziness, or increased sun sensitivity can occur. It’s still best to talk to a healthcare provider before starting, especially if you have a history of mental health conditions or liver issues.
How long does St. John’s Wort stay in your system after you stop taking it?
The enzyme-inducing effects of hyperforin can last up to two weeks after you stop taking St. John’s Wort. That means your body will still process other drugs faster during this time. If you’re switching to a new medication, especially one with a narrow safety window like warfarin or cyclosporine, wait at least 14 days after stopping St. John’s Wort before starting the new drug-and monitor closely.
Are all St. John’s Wort supplements the same?
No. The amount of hyperforin-the main culprit behind drug interactions-varies wildly between brands. Some contain less than 0.1%, others over 3%. There’s no standardization in the U.S., and labels often don’t list hyperforin content. Even "standardized" extracts can be misleading. If you’re taking any medication, avoid St. John’s Wort entirely rather than trying to find a "safer" version.
Can I take St. John’s Wort with vitamins or fish oil?
Most vitamins and fish oil don’t interact with St. John’s Wort. However, if you’re taking vitamin K, it can affect how warfarin works-and if St. John’s Wort is also lowering warfarin levels, the combination becomes unpredictable. Stick to simple supplements if you’re using St. John’s Wort, but again: if you’re on any prescription drug, avoid it completely.
Why don’t more doctors warn patients about this?
Many doctors don’t ask about herbal supplements because patients don’t volunteer the information. Studies show over 70% of patients don’t mention herbal products unless directly asked. Also, time constraints in appointments mean some providers assume supplements are harmless. But the data is clear: St. John’s Wort is one of the most dangerous herb-drug interactions in modern medicine. Always disclose everything you take-no matter how "natural" it seems.
Irving Steinberg
November 28, 2025 AT 21:34bro i took this stuff with my birth control and now im pregnant lmao 🤦♂️
Kay Lam
November 30, 2025 AT 20:16I understand why people reach for St. John’s Wort because modern medicine feels cold and transactional but the truth is that nature doesn’t care about your intentions if you’re on warfarin or cyclosporine your body doesn’t distinguish between a pill and a plant it just sees chemistry and it responds with life or death consequences. This isn’t about being paranoid it’s about respecting how powerful these interactions are. I’ve seen too many people think they’re being smart by going natural and end up in the hospital because they didn’t tell their doctor. The supplement industry thrives on ambiguity and your health shouldn’t be a gamble.
Matt Dean
December 1, 2025 AT 05:58Anyone who takes St. John’s Wort with SSRIs deserves what they get. Serotonin syndrome isn’t a side effect it’s a consequence of being reckless with your brain chemistry. You want to feel better go to therapy get sunlight stop pretending a herb is a cure-all. This isn’t 1998 anymore we have data. Stop being a walking drug interaction.
Walker Alvey
December 2, 2025 AT 17:39Oh so now natural means dangerous but pharmaceuticals are sacred huh? Funny how the same people who scream about Big Pharma are fine with herbal magic that has zero oversight. The real problem isn’t St. John’s Wort it’s that we let people think biology is a choose your own adventure book. You don’t get to pick which rules apply to your liver.
Adrian Barnes
December 3, 2025 AT 12:29The data presented here is unequivocal and the clinical implications are severe. The induction of CYP3A4 and CYP2C9 enzymes by hyperforin results in a pharmacokinetic alteration that compromises the therapeutic index of multiple life-sustaining medications. The anecdotal reports of organ rejection and stroke are not outliers they are predictable outcomes of an underappreciated pharmacodynamic mechanism. Furthermore the lack of standardization in supplement manufacturing renders any dosage assumption statistically invalid. It is not merely prudent to avoid this compound it is a medical imperative for any patient on a narrow-therapeutic-index drug. The failure of healthcare providers to systematically screen for herbal supplement use constitutes a systemic deficiency in patient safety protocols.
Souvik Datta
December 3, 2025 AT 21:27Look I get it. You want something gentle. Something that feels like it’s helping without a prescription label. But here’s the thing - if you’re on meds your body isn’t playing games. It’s doing math. And St. John’s Wort? It’s the cheat code that breaks the whole system. I’ve coached people through depression for years. The real win isn’t finding a magic herb. It’s finding a routine - walking every morning, talking to someone who listens, getting light in winter. Those things don’t come with warning labels. They don’t require blood tests. And they don’t make your transplant fail. You don’t need to be brave to avoid this. You just need to be smart. And if you’re already taking it? Don’t panic. But do talk to your doctor. Slowly. Carefully. And tell them everything. Your life might depend on it.