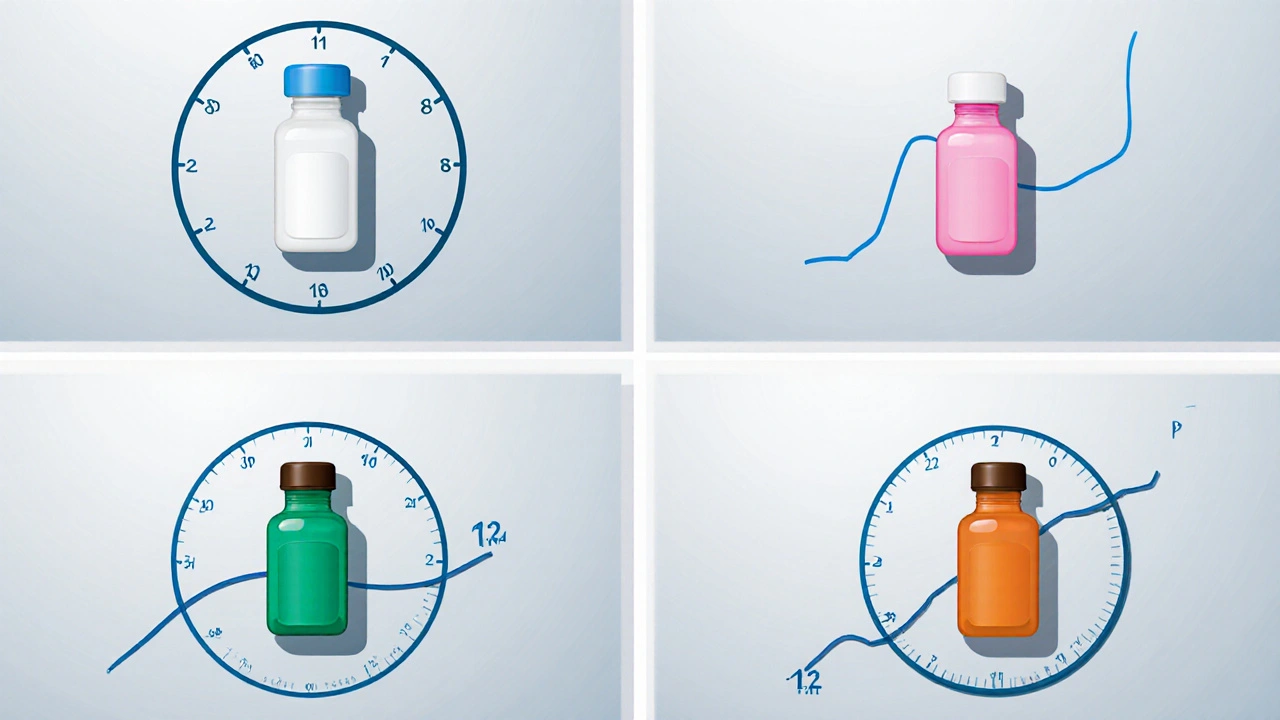
Insulin Cost Comparison Tool
Compare Basal Insulin Costs
Get a clear picture of how much different insulin options cost based on your specific needs and insurance coverage.
Your Information
Insulin Options
Insulin Glargine (Lantus, Basaglar)
$28024-hour flat profile, once daily
Insulin Detemir (Levemir)
$21012-24 hour duration, once or twice daily
Insulin Degludec (Tresiba)
$360Up to 42 hours, flexible timing
NPH Insulin
$75Older option, shorter duration with peak
Key Takeaways
- Insulin Glargine offers a flat 24‑hour profile with once‑daily dosing, making it a solid first‑line basal option.
- Insulin Detemir can be given once or twice daily and is slightly cheaper, but its duration is shorter.
- Insulin Degludec provides an ultra‑long effect (up to 42hours) and flexible timing, though it carries a higher price tag.
- NPH insulin is the cheapest basal but has a pronounced peak and higher hypoglycemia risk.
- Choosing the right basal insulin depends on lifestyle, insurance coverage, and how your body reacts to each formulation.
If you're juggling blood‑sugar numbers and wondering whether Insulin Glargine is right for you, you’re not alone. Below we break down what makes this long‑acting analogue tick, how it stacks up against its most common siblings, and what practical factors-like cost or dosing flexibility-should tip the scales.
What is Insulin Glargine?
When doctors talk about basal insulin, Insulin Glargine is a recombinant human insulin analogue that forms micro‑precipitates under the skin, releasing a steady dose of insulin over roughly 24hours. It was first approved by the FDA in 2000 and is marketed under brand names such as Lantus and Basaglar. Its flat action curve means you generally won’t feel a noticeable “peak,” which reduces the chance of late‑night lows.
How the Main Basal Insulins Differ
Basal insulins fall into two camps: traditional intermediates (like NPH) and modern analogues (Glargine, Detemir, Degludec). The table below captures the biggest practical differences.
| Attribute | Insulin Glargine | Insulin Detemir | Insulin Degludec | NPH Insulin |
|---|---|---|---|---|
| Onset | 1-2h | 1-2h | 1h | 2-4h |
| Peak | None (flat) | Minimal | None (flat) | 4-12h |
| Duration | ≈24h | ≈12-24h (dose‑dependent) | ≈42h | ≈12-16h |
| Dosing Frequency | Once daily | Once or twice daily | Once daily (flexible timing) | Once or twice daily |
| Typical Dose Range (U/kg) | 0.1-0.5 | 0.1-0.5 | 0.1-0.5 | 0.1-0.4 |
| FDA Approval Year | 2000 | 2005 | 2015 | 1950 (original) |
| Average Wholesale Price (2025 US$ per 10mL) | $280 | $210 | $360 | $75 |
| Risk of Severe Hypoglycemia | Low | Low‑moderate | Very low | Higher |
When Insulin Glargine Shines
Because its action is flat, Glargine is a natural fit for people who need a “once‑and‑done” basal dose. If you have a regular daily schedule and can inject at roughly the same time each night, you’ll likely see stable fasting glucose and fewer surprises at breakfast.
Patients with Type 1 Diabetes who run a pump often keep Glargine as a backup in case the pump fails. Its predictable profile makes it easy to calculate a safe “catch‑up” dose.
Insurance plans that list Lantus or Basaglar on their formulary usually cover them at a modest copay, especially under Medicare PartD. For those on a tight budget, the biosimilar Basaglar often costs 10‑15% less than the original brand.
Who Might Prefer Insulin Detemir?
Detemir’s slightly shorter duration can be a blessing if you need flexibility. Some clinicians prescribe it twice daily for patients who experience nocturnal hypoglycemia with Glargine. The molecule binds to albumin, which slows its clearance but also means the effect can wobble a bit with changes in protein levels.
Cost‑conscious patients often gravitate toward Detemir because many generic versions are cheaper than Glargine biosimilars, especially in European markets where the National Health Service negotiates lower prices.
Why Some Choose Insulin Degludec
Degludec’s ultra‑long action (up to 42hours) gives you a wide dosing window. Miss a dose? You can inject up to 24hours later without losing control. This flexibility is prized by shift workers, frequent travelers, and people with erratic sleep patterns.
The trade‑off is price. Even the cheapest degludec product sits near $360 per 10mL, which many US insurers still consider “high‑tier.” If you have premium coverage or qualify for manufacturer assistance programs, the flexibility may be worth it.
NPH: The Old‑School Option
For decades, NPH (neutral protamine Hagedorn) was the go‑to basal insulin. It’s cheap-often under $75 per vial-but its pronounced peak can cause mid‑night lows, especially if you’re active late at night.
Some clinicians still prescribe NPH for patients who can time meals around its peak, or for those who simply cannot afford analogues. If you’re on a strict budget, pairing NPH with a rapid‑acting insulin for meals can be an effective, low‑cost regimen.

How to Switch Safely
- Check your current regimen. Note the total daily basal dose, timing, and recent HbA1c values (the A1C test that measures average glucose over three months).
- Consult your prescriber. They’ll calculate an equivalent dose for the new insulin, usually starting 80‑90% of the old basal dose to avoid hypoglycemia.
- Pick a consistent injection time. For Glargine and Degludec, pick a time you can stick to most days. For Detemir, you may split the dose (e.g., morning and bedtime) based on your glucose pattern.
- Monitor glucose closely. Check fasting glucose each morning for the first two weeks. If you see lows <70mg/dL, reduce the dose by 10‑20%.
- Adjust as needed. After 2-4weeks, review your A1C and time‑in‑range (percentage of readings between 70‑180mg/dL). Fine‑tune the dose or timing before making another switch.
Remember, every body reacts differently. Some people feel the same after a switch; others need a few tweaks. Patience and close communication with your diabetes care team are key.
Real‑World Cost Snapshot (2025)
Below is a quick look at the average wholesale price (AWP) for a standard 10mL vial in the United States. Prices vary by country, insurance, and manufacturer rebates.
- Insulin Glargine (Lantus/Basaglar): $280
- Insulin Detemir (Levemir): $210
- Insulin Degludec (Tresiba): $360
- NPH (Humulin N): $75
In the UK, the NHS typically supplies Glargine or Detemir at a standard tariff of about £20 per vial, while degludec is reserved for specialty cases due to higher cost.
Bottom Line: Which Basal Insulin Fits You?
- Insulin Glargine - Best for steady, once‑daily dosing and when you want a low hypoglycemia risk.
- Insulin Detemir - Good if you need flexibility in timing or want a slightly cheaper analogue.
- Insulin Degludec - Ideal for irregular schedules, shift work, or if you value a “forgive‑me‑if‑I‑miss‑a‑day” profile.
- NPH - Suitable only when cost is the overriding factor and you can manage its peak.
Talk with your endocrinologist, check your insurance formulary, and consider your daily routine. The right basal insulin can smooth out your glucose curve, reduce daily hassles, and keep you feeling more like yourself.
Frequently Asked Questions
Can I mix Insulin Glargine with rapid‑acting insulin in the same syringe?
No. Glargine’s formulation is designed to form a subcutaneous depot. Mixing it with other insulins can alter its absorption and lead to unpredictable glucose drops.
Do I need to refrigerate Insulin Glargine after opening?
Yes, store it in the fridge (2‑8°C). Once in use, you have 28days at room temperature before discarding.
Why does my fasting glucose swing more with NPH than with Glargine?
NPH peaks 4-12hours after injection, often hitting low levels overnight. Glargine’s flat profile avoids that peak, keeping fasting numbers steadier.
Is insulin degludec safe for pregnancy?
Current guidelines list degludec as a Category C drug. It’s not the first choice; most clinicians stick with Glargine or Detemir, which have more extensive safety data in pregnancy.
How often should I check my A1C after switching basal insulin?
Give the new insulin at least three months to show its effect, then repeat the A1C test. Earlier finger‑stick logs help fine‑tune dosing before the lab result.
Joshua Ardoin
October 15, 2025 AT 05:46Hey folks, thanks for sharing this super detailed rundown! 🌟 It’s awesome to see the price breakdown side‑by‑side with the dosing info – makes the whole decision‑making thing way less scary. I’ve been on Glargine for a couple of years and the once‑daily shot really fits my busy schedule, plus the flat profile means fewer middle‑night surprises. If anyone’s juggling a tight budget, the Basaglar biosimilar can shave a decent chunk off the monthly bill without dropping the effectiveness. And hey, don’t forget to double‑check your insurance tier – sometimes a little tweak there can save you more than you think. 🙌
Meigan Chiu
October 16, 2025 AT 09:33While the post is indeed comprehensive, there are a few inaccuracies that need clarification. First, the table lists the average wholesale price for NPH at $75, but recent CMS data shows it hovering around $68 per 10 mL vial. Second, stating that “Insulin Detemir can be given once or twice daily” ignores the fact that many clinicians now prefer a strictly once‑daily regimen for patients with stable fasting glucose. Finally, the claim that “Glargine offers a flat 24‑hour profile” is technically misleading; a slight peak can appear around 8‑12 hours in some individuals. Accuracy matters, especially when patients are making costly choices.
Patricia Hicks
October 18, 2025 AT 17:06Choosing a basal insulin is rarely a one‑size‑fits‑all decision, and the nuances become especially important when you factor in lifestyle, comorbidities, and insurance coverage. First, the pharmacokinetic profile of each analogue dictates not only how often you inject but also how predictable your fasting glucose will be from day to day. Glargine’s near‑flat 24‑hour curve is prized for its simplicity, yet some patients still report dawn‑phenomena spikes that require a slight dose adjustment in the evening. Detemir, on the other hand, offers a slightly shorter duration, which can be an advantage for those who experience nocturnal hypoglycemia, but it may necessitate a split‑dose schedule for optimal control. Degludec pushes the envelope with up to 42 hours of action, granting a generous dosing window that can accommodate shift work or travel, though the premium price can be a barrier for many. NPH remains the budget‑friendly option, but its pronounced peak around 6–10 hours post‑injection means you must be vigilant about timing meals and snacks to avoid lows. Moreover, the real‑world cost differences are amplified by pharmacy rebates, manufacturer assistance programs, and regional pricing variations, so the headline $280 vs $75 figure often hides a more complex picture. For patients on Medicare Part D, formulary placement can dramatically affect out‑of‑pocket expenses, especially when a brand‑name product is tier‑1 versus a biosimilar sitting in tier‑2. Clinical guidelines suggest starting with the most convenient, once‑daily analogue for newly diagnosed type 1 patients, then individualizing based on glucose patterns, hypoglycemia risk, and personal preference. It’s also worth noting that renal impairment can alter insulin clearance, sometimes favoring a shorter‑acting basal like Detemir to reduce the risk of accumulation. Psychological factors shouldn’t be ignored either; the confidence that comes with a predictable insulin curve can improve adherence and overall quality of life. When switching between basals, a prudent strategy is to reduce the initial dose to about 80 % of the previous total basal dose and titrate cautiously while monitoring fasting sugars. Communication with your endocrinologist is essential, as they can anticipate potential gaps in coverage and suggest patient‑assistance resources. In practice, many clinicians find that a hybrid approach-using a cheap NPH in the morning and a longer‑acting analogue at night-balances cost and control, though it adds complexity. Ultimately, the best choice is the one you can afford, stick to consistently, and that keeps your A1C in the target range without frequent lows. So, weigh the pharmacology, the price, and your daily routine before settling on a single basal insulin.
Quiana Huff
October 21, 2025 AT 00:40🚀 Let’s break down the pharmacodynamics: Glargine forms micro‑precipitates that sustain a basal insulin flux, while Detemir’s albumin‑binding domain modulates its half‑life, and Degludec’s multi‑hexamer chain extends the release window up to 42 h. From a formulary perspective, tier‑placement drives the net price per unit, so a high‑tier classification can nullify the clinical benefits of an ultra‑long‑acting analogue. Remember to audit your copay accumulator; some PBMs reset after a certain threshold, which can flip the cost calculus mid‑year. Bottom line: match the insulin’s kinetic envelope to your circadian rhythm and insurance tier for optimal cost‑effectiveness. 😊
William Nonnemacher
October 22, 2025 AT 04:26Too much jargon, not enough clarity.
Alex Ramos
October 24, 2025 AT 12:00Indeed, the data presented in the original post warrants a more nuanced analysis; the price differentials are not merely nominal figures, they reflect systemic pricing strategies, contractual rebates, and manufacturer assistance programs; consequently, a superficial “cheapest is best” mantra overlooks the multifaceted nature of insulin economics, which, in turn, influences patient adherence and therapeutic outcomes.
Mita Son
October 25, 2025 AT 15:46Wow, that riiiight there is the truth! I’m like “whoa” when i see the numbers-yeah, insulin isn’t cheap, but the way they hide the REAL cost? It’s like a drama series, but we’re the ones paying the bill. lol
Richard Walker
October 27, 2025 AT 22:20I appreciate the thorough breakdown; it gives a clear picture of how each basal option fits different lifestyles and budgets.
Jason Oeltjen
October 29, 2025 AT 02:06Honestly, people shoudl read this and stop seeking cheap hacks that end up hurting them in the long run.
Mark Vondrasek
October 31, 2025 AT 09:40Oh sure, because when I think “optimal diabetes management,” the first thing that comes to mind is comparing the price of a vial of insulin to my Netflix subscription. It’s not like I have to worry about hypoglycemia at 3 am or the anxiety of a missed dose. And who cares about the pharmacokinetic nuances when you can just pick whichever one fits your budget-after all, health is just a number on a chart, right? The article does a decent job laying out the facts, but let’s not forget that the real cost includes the sleepless nights and endless doctor visits. If you’re lucky enough to have a generous insurance plan, congratulations, you get to enjoy the luxury of choice. For the rest of us, it’s a balancing act between what we can afford and what keeps our blood sugar from swinging like a pendulum. The take‑home message? Do the math, talk to your provider, and maybe, just maybe, don’t let the pharmacist’s smile distract you from the price tag.
Joshua Agabu
November 1, 2025 AT 13:26Sounds like a good plan-keep an eye on both cost and blood sugar.
Matthew Bates
November 3, 2025 AT 21:00While the preceding discussion offers valuable insights, it is imperative to underscore that any therapeutic decision should be predicated upon a comprehensive assessment of the patient’s clinical profile, concomitant medications, and the prevailing evidence‑based guidelines. Moreover, the economic analysis presented must be contextualized within the framework of regional pricing disparities and insurance formularies to avoid oversimplification.