Fournier's Gangrene Emergency Symptom Checker
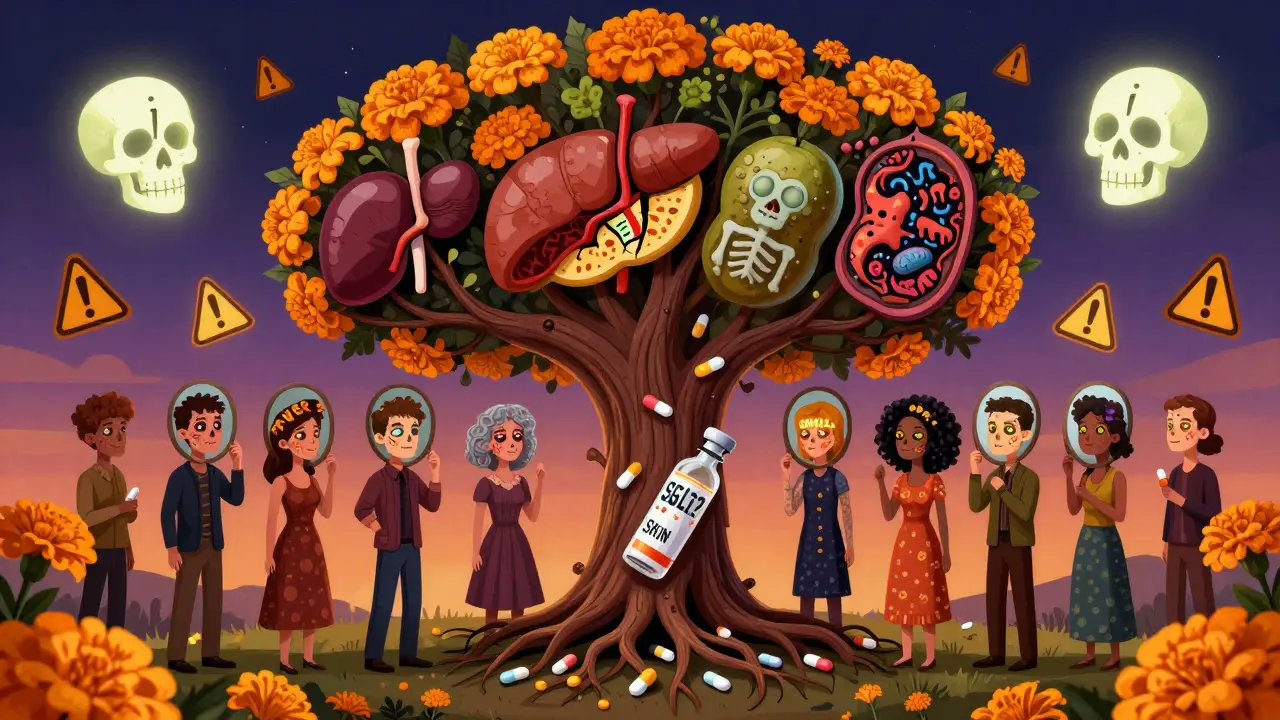
This tool checks for emergency signs of Fournier's gangrene, a rare but life-threatening condition linked to certain diabetes medications. Do NOT use this as medical advice.
If you experience ANY of these symptoms, seek emergency care immediately. Time is critical.
Critical Symptoms:
Imagine waking up with sudden, unbearable pain in your groin or between your legs. It doesn’t feel like a rash or a minor infection. It feels like something is eating away inside you. Your skin is red, swollen, and hot to the touch. You have a fever. You feel sick. And then you notice a foul smell coming from the area. This isn’t a nightmare. It’s Fournier’s gangrene-a rare, fast-moving bacterial infection that destroys tissue in the genitals and anal region. And it’s now linked to certain diabetes medications millions of people take every day.
What Is Fournier’s Gangrene?
Fournier’s gangrene is a type of necrotizing fasciitis. That means bacteria invade the deep layers of skin and tissue, killing them rapidly. It usually starts in the perineum-the area between the genitals and anus-but can spread to the abdomen, thighs, or even the chest. The infection eats through fascia, the connective tissue that holds muscles and organs in place. Without emergency treatment, it kills. It’s not common. But when it happens, it’s brutal. About 1 in 10,000 men taking certain diabetes drugs develop it. Women are getting it too-something doctors didn’t see much of before. The mortality rate? Up to 50% if treatment is delayed. Even with quick action, many patients need multiple surgeries, spend weeks in intensive care, and lose parts of their genitals or skin. Survivors often face long-term physical and emotional scars.Which Diabetes Medications Are Linked to It?
The link was confirmed by the U.S. Food and Drug Administration (FDA) in 2018. Since then, regulators in the UK, New Zealand, and across Europe have updated warnings. The drugs involved are called SGLT-2 inhibitors. They work by making your kidneys flush out extra sugar through urine. That sounds good for lowering blood sugar-but it creates a sticky, sugary environment where bacteria thrive. These medications include:- Canagliflozin (Invokana)
- Dapagliflozin (Farxiga)
- Empagliflozin (Jardiance)
- Ertugliflozin (Steglatro)
Why Do These Drugs Increase the Risk?
It’s not magic. It’s biology. SGLT-2 inhibitors cause glucose to spill into your urine. That sugar doesn’t just disappear-it stays in the urethra, around the genitals, and near the anus. Bacteria love sugar. Yeast, E. coli, and other nasty bugs multiply fast in that warm, moist, sugary mess. What starts as a simple yeast infection or urinary tract infection can turn into a full-blown infection that burrows deep into tissue. People with diabetes already have weaker immune systems. High blood sugar slows healing and makes infections harder to fight. Add the sugary urine from these drugs, and you’ve got a perfect storm. A small cut, a scratch, or even friction from clothing can let bacteria slip under the skin. From there, they spread like wildfire.
Emergency Signs: Don’t Wait, Don’t Doubt
If you’re taking one of these drugs, know these warning signs. They don’t always come slowly. Sometimes, pain hits like a lightning strike.- Severe pain in the genitals, anus, or inner thighs-worse than you’d expect from the visible symptoms
- Redness, swelling, or warmth in the area, spreading quickly
- Fever or chills, even if you feel fine otherwise
- Foul-smelling discharge from the genital or anal area
- Dark, bruised, or dead-looking skin-it might look black or purple
- Malaise-a deep, overwhelming feeling of being seriously ill
What Happens If You’re Diagnosed?
Time is everything. Every hour counts. Once Fournier’s gangrene is suspected, doctors must act fast:- Stop the SGLT-2 inhibitor immediately-no exceptions
- Start strong IV antibiotics-often a mix of drugs to cover multiple bacteria
- Emergency surgery-to cut away dead tissue. Many patients need multiple surgeries over days or weeks
- Intensive care-nearly 80% of cases require ICU admission
- Close blood sugar monitoring-stopping the drug can cause blood sugar to spike, so insulin or other meds may be needed
Who’s Most at Risk?
It’s not just about the drug. Risk goes up with:- Being male (though women are getting it too-about one-third of cases now)
- Having type 2 diabetes for many years
- Being overweight or obese
- Having a history of genital infections
- Being over 65
- Having poor circulation or nerve damage from diabetes
Should You Stop Taking Your Medication?
No-not without talking to your doctor. These drugs save lives. They cut heart attack risk. They protect kidneys. For many, the benefits far outweigh the risk. Fournier’s gangrene is rare. You’re more likely to be struck by lightning than get it. But if you’re taking one of these drugs, you need to be alert. Talk to your doctor about your personal risk. If you’ve had repeated yeast infections or UTIs since starting the medication, that’s a signal. Your doctor might switch you to a different class of drug-like metformin, GLP-1 agonists, or insulin-depending on your health. Never stop cold turkey. Stopping suddenly can cause dangerous blood sugar spikes.What to Do Right Now
If you’re on an SGLT-2 inhibitor:- Know the signs. Print them out. Show them to your partner or family.
- Check your genital area daily, especially if you’re prone to infections.
- Call your doctor if you notice any redness, swelling, or unusual discharge-even if it seems mild.
- If pain is severe, fever is high, or skin looks dark-go to the ER. Don’t wait. Don’t call ahead. Just go.
- Ask your doctor: “Is this drug still right for me?” Review your options every 6-12 months.
Joanne Smith
December 27, 2025 AT 00:27So let me get this straight-my diabetes med is basically a sugar-coated landmine for my private parts? Thanks, Big Pharma, for turning my insulin regimen into a horror movie. I’m just glad I read this before my next yeast infection turned into ‘Fournier’s Revenge.’
Prasanthi Kontemukkala
December 28, 2025 AT 13:57This is such an important post. I’m a nurse in Mumbai, and I’ve seen patients delay care because they thought it was just a ‘bad rash.’ Please, if you’re on these meds, don’t wait. Even if it feels embarrassing to talk about, your life matters more than pride. Share this with someone you love.
Alex Ragen
December 28, 2025 AT 17:56One cannot help but observe, with a certain existential dread, that modern pharmacology has achieved the paradoxical feat of treating metabolic dysfunction by engineering a micro-environment conducive to necrotic proliferation-thus, the SGLT-2 inhibitors, in their noble pursuit of glycosuria, inadvertently resurrect the medieval specter of gangrene, not as a plague of filth, but as a bureaucratic side-effect footnote. Aesthetic irony, indeed.
Lori Anne Franklin
December 29, 2025 AT 19:12OMG I’m on Jardiance and had a weird burny feeling last week-I thought it was just my undies. I’m gonna call my doc tomorrow. This is wild but also so scary. Thanks for posting this, I would’ve never known!
Bryan Woods
December 30, 2025 AT 08:21Thank you for compiling this information with such clarity. The FDA’s warning and the clinical data are unequivocal: early recognition is the single most effective intervention. While the incidence remains low, the consequences are catastrophic without prompt intervention. This is a public health communication well-executed.
Ryan Cheng
December 30, 2025 AT 11:17For anyone on these meds: don’t panic, but do pay attention. If you’ve had recurring UTIs or yeast infections since starting your drug, that’s your body waving a flag. Talk to your doctor about alternatives-metformin, GLP-1s, even insulin if needed. Your quality of life matters more than sticking to a brand name.
wendy parrales fong
January 1, 2026 AT 11:00It’s scary to think your medicine could hurt you like this. But knowing the signs means you can protect yourself. I’m sharing this with my mom-she’s on Farxiga and doesn’t talk much about her health. She needs to know. Love you, Mom.
Jeanette Jeffrey
January 2, 2026 AT 09:21Oh wow, so now we’re blaming drugs for people who can’t keep their crotch clean? How about washing up after peeing? Or wearing cotton underwear? Or not being a diabetic mess? This is just pharma fear-mongering wrapped in a ‘you’re special’ blanket. Also, why is everyone so obsessed with their genitals?
Shreyash Gupta
January 2, 2026 AT 16:56Wait… so if I pee sugar, bacteria grow? 🤔 But… isn’t that just… normal? Like… we’ve always peed sugar? 😅 So why now? Is this just a marketing thing? 🤨 I’m confused. Also, I’m on Invokana and I’m fine… so maybe it’s just me? 😇
Ellie Stretshberry
January 3, 2026 AT 11:15i just got diagnosed with type 2 last year and started on jardiance… i didnt know any of this. i thought the yeast infections were just me being gross. i’m going to the dr tomorrow. thank you for this. i feel less alone now.
Zina Constantin
January 4, 2026 AT 07:31As someone who grew up in a culture where talking about genital health is taboo, I’m so grateful for posts like this. We need more open conversations-even if it feels awkward. Knowledge is power, and power saves lives. Thank you for breaking the silence.
Dan Alatepe
January 6, 2026 AT 00:02Bro… I’m on Farxiga and last week I woke up screaming because my junk felt like it was on fire… I thought I was dying. Went to ER. They said ‘yeast.’ I said ‘no, this is different.’ They gave me cream. I’m still scared. This post… it’s like they read my mind. I’m telling my whole family. This ain’t normal. 🙏
Angela Spagnolo
January 7, 2026 AT 01:56I’m so glad someone finally wrote this clearly… I’ve been scared to say anything because I didn’t want to sound dramatic… but the pain was… wrong. Like, ‘I’m going to die’ wrong. I stopped the drug, got surgery, and now I’m healing. Please, if you’re reading this and feel something off-GO. Just go. Don’t wait.