Antidepressant Tapering Calculator
Create Your Tapering Plan
Important Information
Tapering is crucial to avoid discontinuation syndrome. Short half-life medications like Paroxetine and Venlafaxine require slower tapers (8+ weeks) compared to longer half-life drugs like Fluoxetine.
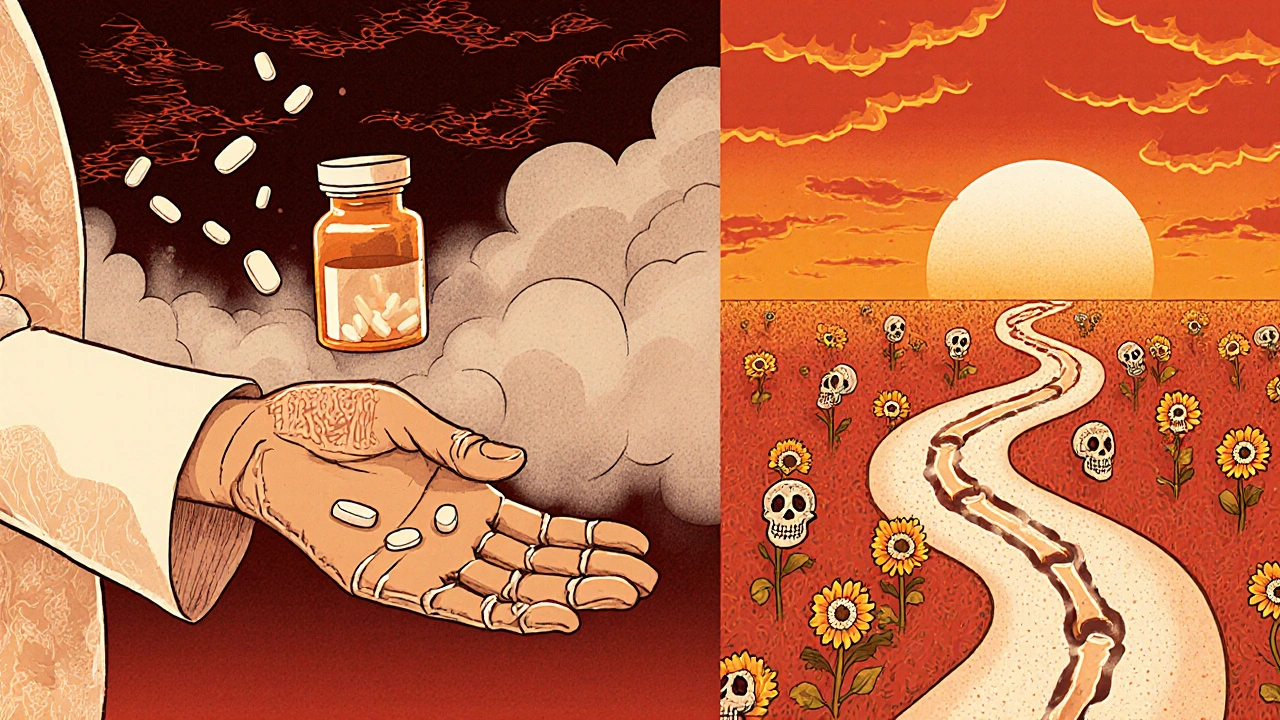
Stopping antidepressants isn’t as simple as just skipping a pill. For many people, the body doesn’t adjust overnight - and when it doesn’t, antidepressant discontinuation syndrome can hit hard. You might feel like you’re falling apart: dizzy, nauseous, buzzing with electric shocks in your head, or overwhelmed by anxiety you didn’t have before. It’s not relapse. It’s not weakness. It’s your nervous system reacting to the sudden absence of a drug your body learned to depend on.
What Exactly Is Antidepressant Discontinuation Syndrome?
Antidepressant discontinuation syndrome, sometimes called withdrawal, happens when you reduce or stop taking an antidepressant after using it for at least a month. It’s not addiction - you won’t crave the drug or use it to get high. But your brain did adapt. Over weeks or months, it changed how it produces and uses serotonin, norepinephrine, and other chemicals to work with the medication. When you take the drug away, those adjustments don’t flip back instantly. The result? A physical reaction that feels very real - and very scary.
Doctors started calling it "discontinuation syndrome" instead of "withdrawal" decades ago, partly to avoid stigma. But experts like Dr. David Healy argue it’s a classic withdrawal syndrome - just one that’s often misunderstood. The American Academy of Family Physicians confirmed its existence in 2006, and since then, studies have shown it affects a significant number of people. The NHS, Mayo Clinic, and Royal College of Psychiatrists all agree: if you’ve been on an antidepressant for more than a month, don’t stop cold turkey.
The Symptoms: What to Watch For
The most common symptoms cluster around six areas - easy to remember with the mnemonic FINISH:
- Flu-like symptoms: Fatigue, muscle aches, chills, headaches, diarrhea
- Insomnia: Trouble sleeping, vivid dreams, or waking up in a panic
- Nausea: Feeling sick to your stomach, sometimes vomiting
- Imbalance: Dizziness, vertigo, unsteady walking
- Sensory disturbances: "Brain zaps" - sudden, brief electric shock feelings in the head, especially when moving your eyes
- Hyperarousal: Anxiety, irritability, agitation, restlessness
Other symptoms are just as common but less talked about: a "cotton wool" feeling in your head, trouble concentrating, derealization (feeling like the world isn’t real), sudden mood swings, anger outbursts, or even suicidal thoughts. These aren’t signs you’re getting worse - they’re signs your brain is recalibrating.
One of the most confusing parts? These symptoms can feel exactly like your original depression or anxiety. That’s why so many people think they’re relapsing - and go back on medication thinking they need a higher dose. But if symptoms started within days of stopping, and they improve within hours of taking a dose again, it’s likely discontinuation syndrome - not relapse.
Which Antidepressants Cause the Worst Withdrawal?
Not all antidepressants are equal when it comes to withdrawal. The biggest factor? Half-life - how long the drug stays in your system.
Short half-life drugs leave your body fast. That means symptoms hit harder and sooner. These include:
- Paroxetine (Paxil): Often called the worst offender. Half-life: about 21 hours.
- Venlafaxine (Effexor): An SNRI. Half-life: 5-11 hours. Nearly half of users report moderate to severe withdrawal.
- Escitalopram (Lexapro): Shorter than fluoxetine. Withdrawal can be intense.
Long half-life drugs leave slowly. That gives your brain more time to adjust:
- Fluoxetine (Prozac): Half-life of 4-6 days. Often used to help others taper off harder drugs because it lingers.
- Fluvoxamine: Also has a longer presence in the bloodstream.
Tricyclics (like amitriptyline) can cause movement problems - stiff muscles, tremors, balance issues. MAOIs (like phenelzine) are the most dangerous to quit abruptly. They can trigger severe agitation, psychosis, or even catatonia. If you’re on an MAOI, never stop without close medical supervision.
How Long Does It Last?
Most people hear that symptoms last 1-2 weeks. That’s true for many - but not all.
According to the National Institutes of Health, symptoms usually appear within 2-4 days and fade within two weeks. But the Royal College of Psychiatrists and patient communities report something different. In fact, a 2022 study in the Journal of Clinical Psychiatry found that nearly 19% of people had symptoms lasting more than three months. Some report them for over a year.
Why the gap? Medical literature often focuses on short-term studies. Patient forums like Surviving Antidepressants have over 15,000 members who describe protracted withdrawal - symptoms that linger for months. One member wrote: "I had brain zaps for 9 months. No one believed me until I found this group." That’s not rare. It’s underreported.
What makes it worse? Switching between generic brands. Not all versions of the same drug are absorbed the same way. A sudden drop in blood levels - even without stopping - can trigger symptoms. That’s why 22% of cases happen during a pharmacy switch, not a planned stop.
How to Stop Safely: The Right Way to Taper
The single best way to avoid discontinuation syndrome? Don’t stop suddenly. Taper slowly - under medical guidance.
Here’s what works:
- Start with your doctor. Never adjust your dose on your own. Even if you feel fine, your nervous system may not be.
- Use the longest half-life option available. If you’re on paroxetine or venlafaxine, ask if switching to fluoxetine for tapering is possible. Fluoxetine’s long presence helps smooth the drop.
- Taper over weeks - not days. For most SSRIs, a minimum 4-week taper. For venlafaxine or SNRIs, 8 weeks or more. Some people need 3-6 months.
- Reduce in small steps. Cutting by 10-25% every 1-2 weeks is safer than big jumps. Some doctors use liquid formulations or pill splitters for precision.
- Watch for triggers. Pregnancy, stress, illness, or sleep loss can make withdrawal worse. If you’re pregnant, don’t stop without talking to your OB and psychiatrist.
Studies show tapering reduces the risk of severe symptoms by 62%. Abrupt cessation increases it by more than 3 times.

What to Do If Symptoms Hit
If you’ve stopped and symptoms start:
- Don’t panic. This is temporary - even if it feels endless.
- Contact your prescriber immediately. Reintroducing your original medication - even just one dose - often lifts symptoms within 24-72 hours.
- Don’t switch to another antidepressant. That can make things worse. The goal is to stabilize, not replace.
- Support your body. Sleep, hydration, gentle movement (like walking), and reducing caffeine can help. Avoid alcohol.
- Track your symptoms. Write down what you feel, when, and how bad. This helps your doctor decide the next step.
Many people feel dismissed by doctors who say, "It’s just withdrawal, it’ll pass." But if your symptoms are severe, lasting more than two weeks, or interfering with daily life - insist on a plan. You’re not overreacting. Your nervous system is healing.
Why This Matters More Than You Think
Antidepressants are prescribed to millions. Yet most patients aren’t warned about discontinuation syndrome before they start. In one Reddit thread with over 1,200 comments, 87% of people said their doctors never mentioned withdrawal. That’s not negligence - it’s systemic ignorance.
But awareness is growing. Clinical trials are now looking for biomarkers to predict who’s at risk. New guidelines are being updated to recognize protracted withdrawal as real. Patients are sharing stories that challenge outdated assumptions.
Stopping an antidepressant isn’t a failure. It’s a transition - and it deserves care, planning, and respect. Your brain didn’t grow dependent on the drug because you were weak. It adapted because it was trying to survive. Now, it needs time to find balance again.
There’s no shame in needing help to do it right. The goal isn’t to stay on medication forever - it’s to leave it safely, without unnecessary suffering.
Can antidepressant withdrawal cause permanent damage?
There’s no evidence that antidepressant discontinuation syndrome causes permanent brain damage. Symptoms are the result of temporary neuroadaptation. Most people fully recover once their nervous system readjusts. However, prolonged symptoms - sometimes lasting months - can feel overwhelming and impact quality of life. This doesn’t mean the damage is permanent, just that healing takes longer than expected. Ongoing research is focused on understanding why some people have protracted withdrawal and how to support them better.
Is it safe to stop antidepressants on my own?
No. Stopping antidepressants without medical supervision increases the risk of severe withdrawal symptoms, misdiagnosis, and relapse. Even if you feel fine, your body may need time to adjust. A doctor can help you create a safe tapering plan based on your medication, dose, and how long you’ve been taking it. Abrupt cessation can lead to dizziness, seizures, or severe mood swings - especially with drugs like venlafaxine or MAOIs.
Why do I get "brain zaps"?
"Brain zaps" are sudden, brief electrical shock-like sensations in the head, often triggered by eye movement. They’re a hallmark of discontinuation syndrome, especially with SSRIs and SNRIs. While the exact cause isn’t fully understood, they’re likely due to changes in serotonin signaling affecting the brainstem and sensory pathways. They’re not dangerous, but they can be startling. They usually fade within days or weeks after restarting the medication or continuing a slow taper.
Can switching to a different antidepressant help with withdrawal?
Sometimes - but only under medical guidance. Switching to a longer-acting antidepressant like fluoxetine can help smooth the transition off a short-acting one. This is called a "cross-taper." But switching randomly or without a plan can worsen symptoms. It’s not a shortcut. It’s a strategy that requires careful timing and monitoring. Never switch medications on your own to avoid withdrawal.
How do I know if it’s withdrawal or a relapse of depression?
Withdrawal symptoms usually start within days of stopping and include physical signs like dizziness, nausea, and brain zaps - things you didn’t have before starting the medication. Relapse symptoms develop more slowly, over weeks, and focus on mood: persistent sadness, loss of interest, hopelessness. If symptoms improve quickly after restarting the original drug, it’s likely withdrawal. If they don’t, it may be relapse. A doctor can help tell the difference.
Are there natural ways to ease withdrawal symptoms?
There’s no proven natural cure, but some strategies can help you feel better while your body adjusts. Prioritize sleep, stay hydrated, eat regular meals, and avoid caffeine and alcohol. Gentle exercise like walking or yoga can reduce anxiety and improve mood. Some people find omega-3s or magnesium helpful, but evidence is limited. The most effective tool remains a slow, supervised taper. Natural remedies don’t replace medical care - they just support it.
Final Thoughts: You’re Not Alone
If you’re going through this, you’re not broken. You’re not crazy. You’re not failing. You’re simply one of millions whose body responded to medication - and now needs time to recalibrate. The medical system has been slow to catch up, but patient voices are changing that. Share your experience. Find your community. Ask for help. And remember: stopping antidepressants isn’t a race. It’s a quiet, careful process - and you deserve to do it right.
John Mackaill
November 22, 2025 AT 17:46Been through this with paroxetine. Thought I was losing my mind-brain zaps every time I turned my head, nausea so bad I couldn’t eat, and this weird buzzing in my chest like my nerves were short-circuiting. My doctor acted like it was ‘just in my head.’ Took me six months to taper, and I still get the occasional zap if I’m stressed. You’re not weak. Your brain just got used to a crutch and now it’s learning to walk again.
Don’t let anyone tell you it’s ‘not real.’ It’s biology, not weakness.
Adrian Rios
November 23, 2025 AT 07:27Let me tell you something that no one talks about in the medical textbooks: switching between generic brands can trigger withdrawal like a goddamn landmine. I was on escitalopram for two years, felt fine, then my pharmacy switched me to a different manufacturer. Three days later, I was dizzy, sweating, and had these electric shocks in my skull like someone was tapping my brain with a live wire. I called my doctor, panicked, and he said, ‘Maybe it’s just anxiety.’ I almost went back on it out of fear.
Turns out, the bioavailability of the generic was off by 12%. That’s enough to destabilize your entire nervous system. This isn’t just about tapering-it’s about regulatory oversight. Why are we letting pharmacies swap meds like they’re swapping toothpaste brands? We need stricter standards. This isn’t anecdotal. It’s systemic.
Casper van Hoof
November 24, 2025 AT 08:27The conceptual framing of antidepressant discontinuation as a ‘syndrome’ rather than ‘withdrawal’ is a semantic maneuver rooted in the pharmaceutical industry’s historical desire to dissociate psychopharmacological agents from the stigma of addiction. While the neurobiological mechanisms are undeniably real-namely, serotonergic downregulation and receptor hypersensitivity-the nomenclature reflects a sociopolitical imperative to preserve the legitimacy of long-term SSRI use. One might argue that the reluctance to acknowledge withdrawal as such stems from the same cognitive dissonance that once denied the addictive potential of opioids. The body adapts; adaptation implies dependence; dependence implies withdrawal. The language must evolve to match the physiology.
Pramod Kumar
November 25, 2025 AT 05:03Man, I remember when I tried to quit venlafaxine cold turkey after a year. Felt like my brain was a radio tuned to static-every thought crackled, my limbs felt like jelly, and I had this phantom buzzing under my scalp like a swarm of bees trapped in my skull. My mom thought I was faking it. My boss thought I was lazy. I didn’t even tell my therapist until I cried in the shower for three days straight.
Then I found a Reddit group called Surviving Antidepressants. That’s where I learned the truth: it’s not you. It’s your damn neurotransmitters throwing a tantrum. I tapered over five months using liquid drops. Took forever. But I’m back. Not ‘cured’-just balanced. And I’m not ashamed to say I needed help to get there. You’re not broken. You’re just recalibrating. Keep going. You got this.
Lisa Lee
November 26, 2025 AT 09:01This is why I hate how America turns every problem into a medical issue. You’re sad? Take a pill. Can’t sleep? Take a pill. Now you can’t quit the pill without turning into a human lightning rod? That’s not science-that’s corporate laziness. My cousin took Prozac for six months and now she’s in a three-year withdrawal spiral. All because some doctor handed her a script like it was candy. We need to stop drugging our feelings and start teaching people how to live with them.
Jennifer Skolney
November 27, 2025 AT 08:35Brain zaps are the worst 😭 I had them for 4 months. I thought I was having mini-seizures. Took me 7 months to taper off Lexapro with my doctor’s help. I cried so hard the first time I didn’t feel dizzy after standing up. You’re not alone. I’m here if you need to vent. 💙
JD Mette
November 28, 2025 AT 03:06I’m not a doctor, but I’ve been on and off antidepressants three times now. The one thing I’ve learned? Tapering too fast is like ripping off a bandage-you think it’ll be quick, but you just make the wound worse. I tried cutting my dose in half after four weeks. Ended up in the ER with vertigo and panic attacks. Took me six more months to recover. Slow is the only way. Even if it feels like you’re moving backward, you’re still moving forward. Just… slower.
Olanrewaju Jeph
November 28, 2025 AT 08:37It is imperative to emphasize that discontinuation syndrome is not a psychological phenomenon but a well-documented neurochemical adaptation. The persistence of symptoms beyond two weeks, particularly in patients discontinuing short-half-life agents such as venlafaxine and paroxetine, is not anomalous but statistically significant. The literature, including the 2022 Journal of Clinical Psychiatry study referenced, demonstrates a clear dose-response relationship between tapering velocity and symptom severity. Therefore, clinical protocols must be revised to mandate individualized tapering schedules, with minimum durations of 12 weeks for high-risk agents. Furthermore, pharmacists must be trained to recognize the clinical implications of generic substitution. This is not a matter of patient compliance-it is a matter of clinical responsibility.