Choosing birth control isn’t just about convenience - it’s about your body, your health, and what you’re willing to live with day after day. The contraceptive patch, the vaginal ring, and the IUD are three popular options, each with very different risks and benefits. If you’re trying to decide which one is right for you, you need real facts - not marketing. Here’s what actually happens when you use these methods, what goes wrong, and who should avoid them.
How Each Method Works
The contraceptive patch (like Xulane®) sticks to your skin and releases hormones - norelgestromin and ethinyl estradiol - into your bloodstream. You change it once a week for three weeks, then go patch-free for a week. It’s designed to mimic the pill, but without having to remember a daily dose.
The vaginal ring (NuvaRing®) is a small, flexible ring you insert yourself. It releases etonogestrel and ethinyl estradiol continuously over three weeks. You take it out for a week, then put in a new one. It works similarly to the patch and pill, but the hormones are absorbed through vaginal tissue instead of the gut.
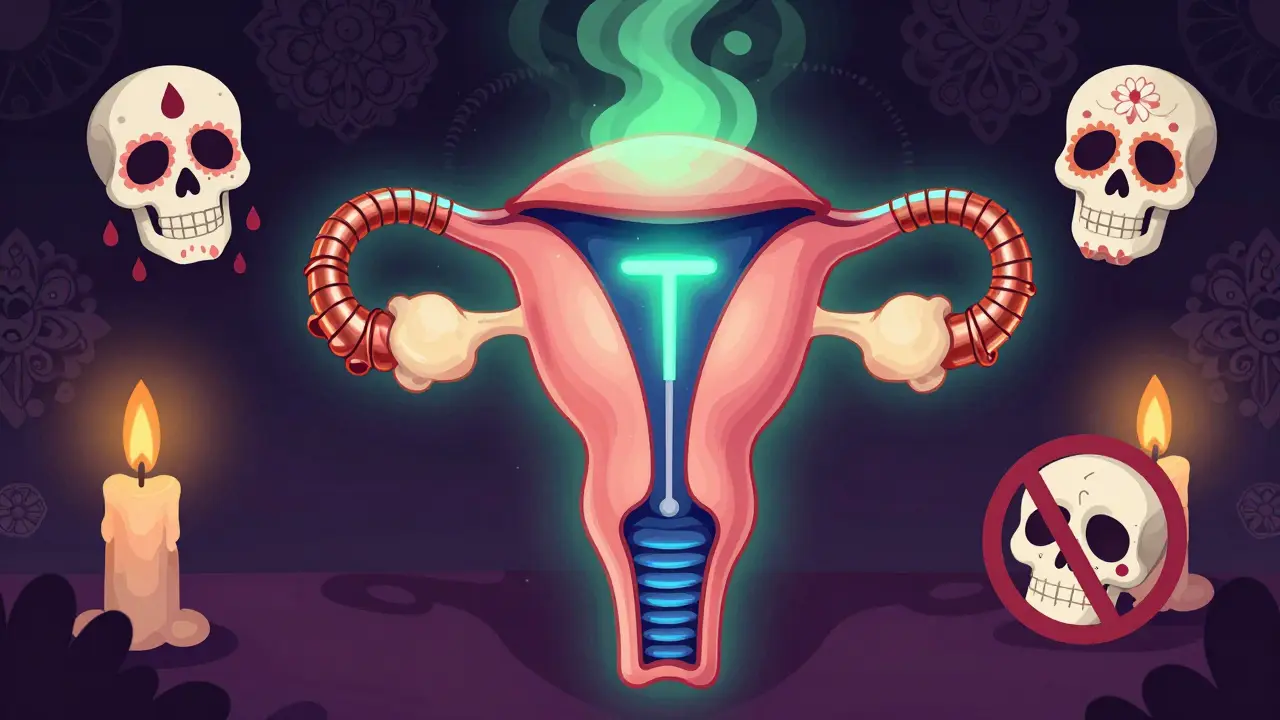
The IUD is completely different. It’s a tiny T-shaped device inserted into your uterus by a provider. There are two types: copper (Paragard®) and hormonal (Mirena®, Liletta®, Kyleena®, Skyla®). Copper IUDs work by releasing ions that are toxic to sperm. Hormonal IUDs release levonorgestrel, which thickens cervical mucus and thins the uterine lining. They last 3 to 12 years depending on the brand, and once inserted, you forget about them.
Efficacy: What Actually Works
It’s easy to think all birth control is equally effective - but it’s not. The patch and ring are both 91% effective with typical use. That means about 9 out of 100 people using them will get pregnant in a year. Why? Because people forget. The patch can fall off. The ring can slip out. Life happens.
IUDs? They’re over 99% effective. Less than 1 out of 100 users gets pregnant. That’s because once it’s in, it’s in. No daily action. No weekly reminder. No risk of forgetting. A 2022 JAMA review found that long-acting methods like IUDs have pregnancy rates of 0.27 per 100 women-years - compared to 4.55 for short-acting methods like the patch and ring.
And if you need emergency contraception? The copper IUD is the most effective option. Inserted within 120 hours of unprotected sex, it reduces pregnancy risk to 0.1% - better than the morning-after pill.
Risks: Blood Clots, Hormones, and What You Might Not Know
Here’s where things get serious. The patch and ring both contain estrogen. Estrogen increases your risk of blood clots - especially in the legs and lungs. A 2022 JAMA review confirmed estrogen-containing methods raise venous thrombosis risk from 2-10 events per 10,000 women-years to 7-10. The patch may be worse than the pill. Some studies suggest women using the patch have a higher risk of clots than those on the pill, even though both deliver the same hormones. Why? Because the patch delivers more estrogen through the skin than the pill does through the gut. The FDA has flagged this concern.
If you smoke, are over 35, have high blood pressure, migraines with aura, or a history of clots - you should avoid the patch and ring. These aren’t just warnings on a leaflet. These are life-threatening risks.
IUDs don’t have this problem. Copper IUDs are completely non-hormonal. Hormonal IUDs release progestin locally - very little enters your bloodstream. That means almost zero risk of blood clots. For women with cardiovascular risks, IUDs are often the only safe hormonal option.

Side Effects: What You’ll Actually Feel
Side effects vary wildly between methods - and not everyone talks about them.
With the patch, skin irritation is common. Around 42% of users report redness, itching, or rash at the application site. Breakthrough bleeding is also frequent - 37% of users in Healthgrades reviews mention it. And yes, the patch can fall off. Studies show 1.8% completely detach, and 2.8% partially detach. If it falls off and you don’t notice, you’re unprotected.
The vaginal ring can cause vaginal discomfort, discharge, or even expulsion during sex. About 3-5% of users report the ring coming out. Some say it’s uncomfortable during intercourse. Breakthrough bleeding is less common than with the patch, but withdrawal bleeding (your period) is often heavier than with the pill.
With copper IUDs, your periods get heavier and cramps get worse. One Medical reports 57% of Paragard users say their periods became unbearable - 8 days of heavy flow, intense cramping, even anemia. But for some, that’s a trade-off they accept for hormone-free contraception.
With hormonal IUDs, it’s the opposite. Most users see lighter periods. After 6-12 months, 20-30% stop getting periods entirely. But in the first few months? Irregular bleeding. Spotting. Days of brown discharge. It’s common. It’s not dangerous. But it can be frustrating.
Cost and Accessibility
Upfront cost matters. The patch costs $15-$80 per month without insurance. The ring? $0-$200. Both add up fast. IUDs cost $0-$1,300 to insert - but that’s a one-time fee. They last 3 to 12 years. Over time, they’re the cheapest option by far.
Access is another factor. Getting an IUD requires a clinic visit. You’ll feel cramping during insertion - sometimes strong enough to make you dizzy. But it takes 5-10 minutes. No surgery. No anesthesia. Just a quick procedure.
Insurance coverage varies. The Affordable Care Act covers birth control, but some insurers still limit patch coverage because of safety concerns. IUDs are almost always covered - and often free.
Who Should Choose What?
Let’s cut through the noise. Here’s who each method works best for:
- Choose the patch if you want hormone-based birth control without daily pills - but you’re young, healthy, don’t smoke, and you’ll remember to change it every week. If you’re active, sweat a lot, or have oily skin, this might not stick.
- Choose the ring if you want something low-maintenance but still hormone-based. You’re okay with monthly insertion/removal and don’t mind a little discomfort. Avoid if you have vaginal infections or have had trouble with expulsion before.
- Choose a copper IUD if you want hormone-free, long-term protection. You’re okay with heavier periods. You’re looking for emergency contraception backup. You want something that lasts 10+ years.
- Choose a hormonal IUD if you want long-term birth control without daily pills - and you’d love lighter or no periods. You have heavy bleeding, cramps, or endometriosis. You have cardiovascular risks and can’t use estrogen.
Experts like the American College of Obstetricians and Gynecologists (ACOG) say IUDs should be first-line for most women. Why? Because they’re the most effective and safest for long-term use. Dr. Jen Gunter says it plainly: “IUDs have the lowest failure rate of any reversible method and don’t carry the blood clot risks associated with estrogen-containing methods.”
What to Do If Something Goes Wrong
If you’re using the patch and it falls off, check the instructions. If it’s been off for more than 24 hours, you need backup contraception for 7 days. If you’re using the ring and it slips out, rinse it with cool water and reinsert. If it’s been out longer than 3 hours, use backup for 7 days.
If you have severe pain after IUD insertion, fever, or foul-smelling discharge, call your provider. These could signal infection or perforation - rare, but serious.
If you develop sudden leg pain, chest pain, trouble breathing, or vision changes - get help immediately. These are signs of a blood clot. Don’t wait. Don’t assume it’s “just a cramp.”
Switching Methods: What You Need to Know
You can switch between methods, but timing matters. Never switch from a hormonal IUD to the patch without waiting. If you remove the IUD and immediately apply the patch, you risk overlapping hormones - which can cause spotting, mood swings, or even increased clotting risk. Wait at least 7 days after removal before starting the patch.
Starting any hormonal method mid-cycle? Use backup contraception (like condoms) for 7 days. Copper IUDs work immediately - even as emergency contraception.
One Medical warns: “Avoid switching to a patch until removal of a hormonal IUD.” This isn’t a suggestion - it’s a safety rule.
The Bottom Line
There’s no single “best” birth control. But there is a safest one - for most people. IUDs win on effectiveness, safety, and long-term cost. The patch and ring are convenient, but they carry higher risks - especially if you have any cardiovascular risk factors.
If you’re young, healthy, and don’t smoke - the patch or ring might work. But if you’re over 35, have migraines with aura, high blood pressure, or a history of clots - skip them. Go for an IUD.
And if you’re unsure? Talk to your provider. Ask: “What’s my risk for blood clots? Do I have any conditions that make estrogen unsafe?” Don’t let convenience override safety. Your body isn’t a lab experiment. It’s your life.
Can the contraceptive patch cause blood clots?
Yes. The patch delivers more estrogen into the bloodstream than the pill, increasing the risk of venous thrombosis. Studies show women using the patch have a higher risk of blood clots in the legs and lungs than those using oral contraceptives, even though both contain similar hormones. The FDA has issued warnings about this risk. Women over 35, smokers, or those with a history of clots should avoid the patch.
Is the IUD safer than the patch or ring?
For most women, yes. IUDs - especially copper and hormonal ones - carry almost no risk of blood clots because they don’t rely on systemic estrogen. Hormonal IUDs release progestin locally, not into the bloodstream. The American College of Obstetricians and Gynecologists recommends IUDs as first-line contraception because they’re more effective and safer long-term than short-acting methods like the patch or ring.
Do IUDs make periods worse?
It depends on the type. Copper IUDs often make periods heavier and cramps worse - up to 57% of users report this. Hormonal IUDs do the opposite: they usually lighten periods, and many users stop having periods after a year. The first 3-6 months with any IUD can involve irregular bleeding or spotting, but that typically improves.
Can I use the ring if I have migraines?
No - if you have migraines with aura. Estrogen in the ring can trigger severe strokes in these cases. Even if your migraines are mild, estrogen-containing methods like the ring and patch are contraindicated. Hormonal IUDs or copper IUDs are safer alternatives. Always discuss your migraine history with your provider before choosing birth control.
How long does it take for an IUD to start working?
Copper IUDs work immediately - even as emergency contraception if inserted within 120 hours of unprotected sex. Hormonal IUDs are effective right away if inserted during your period. If inserted at any other time, use backup contraception (like condoms) for 7 days. The patch and ring take 7 days to become effective if started mid-cycle.
Which method is cheapest long-term?
The IUD. Upfront cost is higher - $0 to $1,300 - but it lasts 3 to 12 years. The patch costs $15-$80 per month. The ring costs $0-$200 per month. Over 5 years, the patch or ring could cost $900-$4,800. An IUD costs less than $300 total over the same period - even with insertion fees.
Camille Hall
February 7, 2026 AT 08:05I’ve been on the hormonal IUD for 3 years now, and honestly? It’s been life-changing. No more PMS rage, no more bleeding through my clothes, and zero worry about forgetting something. The first 3 months were rough-spotting every day like I was in a horror movie-but then it just… stopped. Now I get maybe 2 days of light flow once a year. I didn’t think I’d ever say this, but I’m kinda grateful for cramps now because they mean I’m not pregnant. Also, my partner says he can’t feel it. That’s a win.